Congestive prostatitisis a pathological process in the prostate gland caused by congestion. Pathogenic flora is not detected; microscopy of prostate secretions, sperm and urine may reveal leukocytes. Symptoms include constant pain pain in the perineum, dysuria. Diagnosis is based on the results of bacterial culture of the biomaterial and TRUS. There is no single treatment regimen for congestive prostatitis; massage, physiotherapy, antimicrobial drugs and alpha-blockers are prescribed. An individual approach is required, taking into account the existing symptoms. If conservative treatment fails, surgery is possible.
General information
Prostatitis can be infectious, caused by the presence of pathogenic microflora, or stagnant, associated with blood congestion, ejaculate retention and prostate secretions. Congestive or congestive prostatitis (urogenital vegetative syndrome, prostatosis) is an outdated name. Modern specialists in the field of urology more often use the term "chronic pelvic pain syndrome without inflammatory response" (CPPS). Prostatitis occurs in 25% of men aged 35-60, inflammation caused by congestive processes accounts for 88-90% of the total number of cases. The potentially congestive form of the disease is supported by pathogens that are L-shaped, fixed in biofilms, and undetectable by routine methods.
Causes
The causes of congestive prostatitis can be related to both the gland itself and extraprostatic factors. The exact etiology is unknown, perhaps due to stagnation of secretions in the prostate or it is a consequence of venous congestion in the pelvic organs and scrotum. Some urologists consider the condition to be psychosomatic. The line between bacterial and bacterial inflammation is very arbitrary; with immunosuppression of any origin, due to the addition of secondary microflora, the process becomes infectious. Congestive prostatitis is caused by:
- Internal urological causes. Functional or structural pathology of the bladder: obstruction of the cervix, inability of the external sphincter to relax during bowel movements, impaired contractility of the detrusor contribute to urine retention and, due to compression of the vessels, blood stagnation. Prostatic hyperplasia and tumor, urethral stricture, and obstructive bladder stones are also considered possible causes of venous congestion.
- Compression. Blood circulation is obstructed due to compression of the venous plexus by a retroperitoneal tumor, metastases, and bowel loops filled with feces (constipation). The vessels of the genitourinary plexus expand, blood flow slows down, tissues experience oxygen starvation and are replaced by dysfunctional structures. A part of the blood is deposited and removed from the circulation.
- Behavioral factors. Refusal of sexual activity, irregular ejaculation and the use of interrupted sexual intercourse as a means of preventing unwanted pregnancy cause bleeding and swelling of the prostate tissue. During ejaculation, this gland does not drain completely. Constant masturbation can lead to congestive prostate, because. . . For the development of an erection, a flow of blood to the genitals is necessary.
Predisposing factors include low physical activity, hypothermia and overheating, poor diet with a predominance of spicy, smoked foods. Alcohol and nicotine affect the tone of the vascular wall, disrupt redox processes and permeability, which provokes swelling. The main prerequisites for the formation of congestive prostatitis affecting all organs of the male genital area (vesicles, testicles) are considered to be abnormalities of the vascular system of the pelvis - valvular insufficiency, congenital weakness of the venous wall.
Pathogenesis
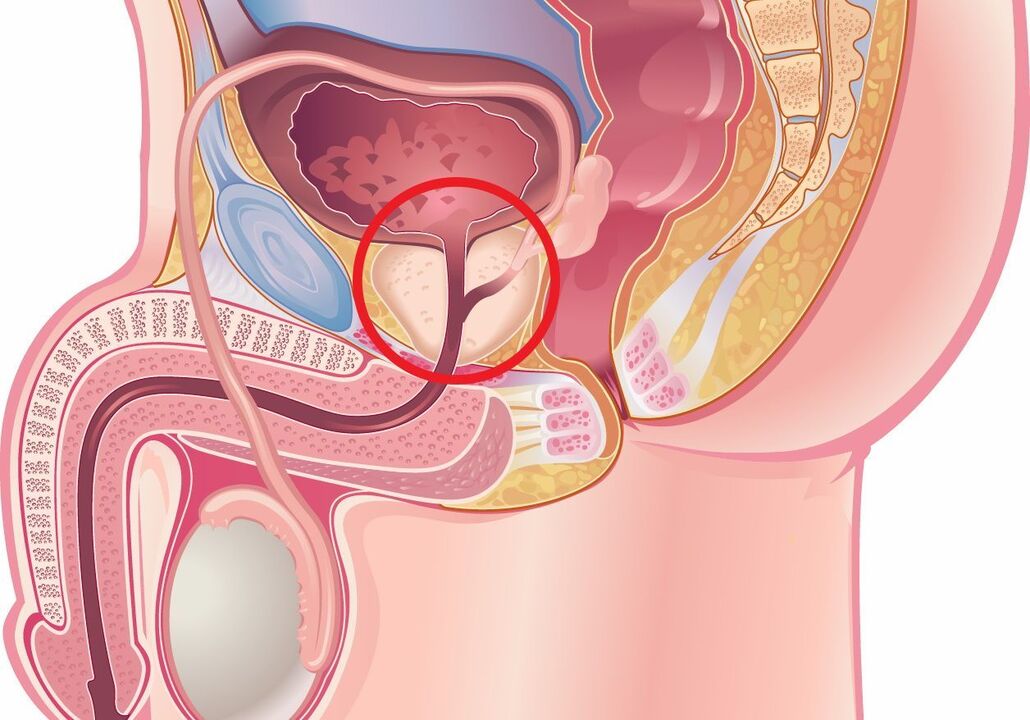
The peripheral area of the prostate gland consists of ducts that have a poorly developed drainage system, which prevents secretions from escaping. As the prostate enlarges with age, patients develop reflux of urine into the prostatic tubes. It has been noticed that many men suffering from prostatitis are more prone to allergies. Scientists believe that such patients may also suffer from autoimmune-mediated inflammation caused by a previous infection.
Urine reflux is caused by urethral strictures, bladder dysfunction and BPH. Backflow of even sterile urine leads to chemical irritation and inflammation. Fibrosis of the tubules begins, preconditions for prostatolithiasis are created, which increases intraductal obstruction and stagnation of secretions. Insufficient drainage of the acini causes an inflammatory reaction, increased swelling is associated with the appearance of symptoms. The condition is aggravated by congestion (stagnation) of blood in the pelvis.
Distribution
The general classification of prostatitis includes acute (I) and chronic (II) bacterial forms. Category III includes subtype IIIa – CPPS with inflammation and IIIb – CPPS without it. Congestive prostatitis is considered a manifestation of CPPS in the absence of an inflammatory response (IIIb). There is a clinical differentiation that takes into account the pathogenetic and morphological features of the disease:
- The first phase.It is characterized by the predominance of processes of exudation, emigration, arterial and venous hyperemia, which results in damage to the microvasculature and destruction of glandular tissue. These changes are registered during the first years from the onset of the disease. The clinical framework in the first stage is more pronounced.
- Second phase.The initial processes of proliferation of connective tissue develop and symptoms decrease. Due to the formation of thrombus, microcirculation suffers, which worsens sclerosis. At this stage, most patients experience sexual dysfunction: erection and orgasm intensity weaken, premature ejaculation develops or, conversely, the man experiences difficulties in reaching climax.
- The third stage. Severe fibrosclerotic changes are typical. It has been proven that proliferation of connective tissue is stimulated not only by inflammation, but also by ischemia accompanying congestive prostatitis. Complaints about difficulty urinating are typical and the involvement of the kidneys in the pathological process is noted.
Symptoms of congestive prostatitis
The pathology is manifested by a number of symptoms. Most patients describe the pain as constant discomfort in the perianal area, scrotum or penis. Some notice increased perineal pain when sitting. The radiation of pain is variable - in the lower back, inner thighs, tail. Swelling of the gland often makes it difficult to urinate and weakens the flow of urine. A congestive type of inflammation against the background of vascular pathology is often accompanied by hemospermia - the appearance of blood in the semen.
Symptoms of bladder irritation include frequent urge to urinate and incontinence. With long-term pathology, depressive disorders develop. It is still debatable whether the psycho-emotional characteristics lead to discomfort in the perineum or, conversely, the pain caused by the swelling of the prostate gland affects the mental state of a man. An increase in temperature with chills indicates the transition from abacterial congestive prostatitis to infectious and the need to start pathognomonic treatment.
Complications
Congestive prostatitis with the addition of microflora can become acute bacterial. Adjacent organs and structures can be involved in the inflammatory process: vesicles, bladder, testicles. The role of the prostate gland is to produce fluids for sperm; normally it has a special composition that has a protective function for male germ cells. Insufficient amounts of nutrients and changes in the biochemical properties of prostate secretions inevitably affect the quality of the ejaculate; men with congestive prostate are more often diagnosed with infertility.
With severe swelling of the organ, part of the urine after urination remains in the bladder, which leads to the formation of pathological reflux of urine in the ureters and in the collecting system of the kidneys. In response to reflux, persistent hydronephrosis and pyelonephritis with impaired renal function may occur. 50% of men develop sexual dysfunction: painful ejaculation, dyspareunia, unpleasant erections at night, which worsens the quality of life and negatively affects the couple's relationship.
Diagnosing
Determining the origin of symptoms is crucial for the effective treatment of congestive prostatitis, therefore various questionnaires have been developed to facilitate the diagnosis: I-PSS, UPOINT. These questionnaires are available in Russified form; they are used by urologists and andrologists in their practice. To exclude myofascial syndrome, consultation with a neurologist is indicated. On palpation, the prostate is enlarged, moderately painful; the congestive nature of the disease is evidenced by the varicose veins of the rectum. The diagnosis of congestive prostatitis includes:
- Laboratory testing. A microscopic and cultural examination of the prostate fluid is performed. A slight increase in the number of leukocytes under the microscope and negative results of bacterial culture confirm abacterial congestive inflammation. PCR tests are performed to exclude the sexually transmitted nature of the disease. In the third part of the urine after the massage, the most pronounced leukocytosis is detected. To rule out a bladder tumor, urine cytology can be performed; in patients over 40-45 years of age, a PSA blood test is justified.
- Visual search methods. The main instrumental diagnostic method remains TRUS, ultrasound of the bladder. The results of cystourethrography are informative for confirming bladder neck dysfunction, detecting intraprostatic and ejaculatory reflux of urine and urethral narrowing. In case of pronounced weakening of the jet, uroflowmetry is performed. Pelvic floor muscle tension is assessed using a videourodynamic study.
Differential diagnosis is made with carcinoma of the bladder, BPH, interstitial cystitis. Similar manifestations are observed in genitourinary tuberculosis and urethral stricture, as these nosologies are also characterized by pain in the lower abdomen, symptoms of dysuria and difficulty urinating. Congestive prostatitis is distinguished from bacterial prostatitis, in addition, all pathological processes associated with CPPS in men must be excluded.
Treatment of congestive prostatitis
The patient is recommended to normalize his sexual life, since regular ejaculation helps drain the acini and improve microcirculation. Interrupted or prolonged sexual intercourse, which provokes congestion, is unacceptable. A number of products have been identified that increase the chemical aggressiveness of urine - their consumption leads to increased symptoms of congestive prostatitis. Spices, coffee, marinades, smoked foods, alcoholic and carbonated drinks should be limited, or better yet excluded. Treatment of congestive inflammation of the prostate gland can be conservative and surgical.
Conservative therapy
The treatment regimen is selected individually, depending on the predominant symptoms. In many patients, improvement occurs after taking antibacterial drugs, which is explained by the incomplete diagnosis of latent infections. For slow urine flow and the need to strain, alpha-blockers are prescribed. Urinary urgency is neutralized with anticholinergic drugs. 5-alpha reductase inhibitors have been shown to reduce the severity of clinical manifestations by reducing the response of macrophages and leukocytes and their migration to the inflammatory site.
Pain relievers, nonsteroidal anti-inflammatory drugs, and muscle relaxants can help relieve muscle pain and spasms. It is reasonable to include in the treatment regimen drugs that normalize microcirculation - phlebotonics (venotonics). If the stagnant process supports androgen deficiency, they use hormone replacement therapy. Patients with anxiety-hypnotic and depressive disorders are advised to consult a psychiatrist who will choose the optimal antidepressant.
With congestive inflammation of the prostate, physiotherapeutic procedures help normalize men's health. They use laser and magnetic therapy, electrophoresis, etc. Treatment at the spa helps to relieve symptoms of dysuria and improve sexual function: taking alkalizing mineral waters, paraffin and mud applications, massage shower. In some patients, the normalization of well-being is observed when performing exercise therapy to reduce tension in the pelvic muscles. Prostate massage does not replace natural ejaculation, but improves blood circulation and drainage of the organ.
Minimally invasive treatment methods
If conservative therapy is unsuccessful, high-tech interventions are considered - transurethral resection of the prostate, high-intensity focused ultrasound ablation. The most effective is transrectal hyperthermia - a non-invasive method based on the principle of thermal diffusion (the prostate is exposed to unfocused microwave energy). Heat increases tissue metabolism, reduces congestive symptoms and has a neuroanalgesic effect. Data on the effectiveness of procedures in the treatment of congestive prostatitis are limited.
Prognosis and prevention
The prognosis for life is favorable, but chronic pelvic pain is difficult to treat. Sometimes congestive prostatitis resolves spontaneously over time. A long-term disorder of blood circulation leads to sclerosis of the tissue of the gland, which is manifested by a deterioration of spermogram parameters. The prognosis for congestive prostatitis depends mainly on the patient's compliance with all recommendations and lifestyle changes.
Prevention includes playing sports, avoiding lifting weights, normalizing sexual relations and avoiding coffee and alcohol consumption. When working sitting, it is recommended to take breaks to do physical exercises and use a pillow. Underwear and loose pants are preferred. Patients are observed by a urologist with periodic assessment of prostate secretions for inflammation and ultrasound and, if necessary, receive antibacterial treatment and prostate massage sessions.




































